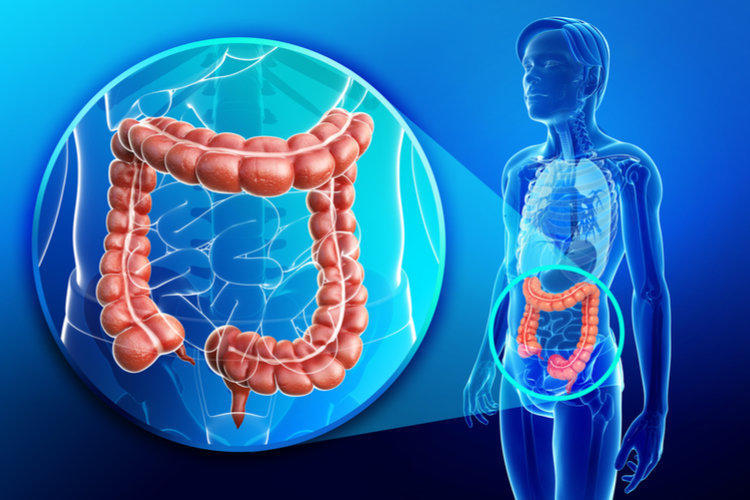
The inflammatory process of the colon is called colitis (from the Greek kolon – the large intestine and itis – the inflammatory process). Inflammatory bowel disease is a general term used to designate a group of chronic pathologies when the disease process affects the digestive tract.
- Ulcerative colitis
- Causes
- Symptoms
- Treatment
- Proctitis
- Total and left-sided colitis
- Surgical treatments for ulcerative colitis
- Forecast
- Crohn’s Disease
- Causes
- Symptoms
- Drug treatment for Crohn’s disease
- Terminal ileocolitis, ileitis
- Crohn’s disease of the colon ─ colitis
- Crohn’s Disease Attack
- Surgical treatment of Crohn’s disease
- Forecast
- Extraintestinal symptoms of chronic colitis
- Microscopic colitis
- Causes
- Lymphocytic Colitis
- Collagen Colitis
- Symptoms of microscopic colitis
- Treatment of microscopic colitis
- Pseudomembranous (infectious) colitis
- Causes
- Symptoms
- Treatment
- Radiation colitis
- Symptoms
- Treatment
- Ischemic Colitis
- Symptoms
- Treatment
Intestinal colitis is a pathology of the colon and rectum. The disease is accompanied by inflammation or degeneration of the inner shell due to an infectious, ischemic, medicinal lesion. These include the following diseases:
- ulcerative colitis (ulcerative colitis);
- Crohn’s disease ─ terminal ileitis, colitis, ileocolitis;
- microscopic colitis ─ lymphocytic and collagen;
- pseudomembranous (infectious) colitis;
- radiation (ray) colitis;
- ischemic colitis.
All colitis has the following manifestations: frequent bowel movements, flatulence, diarrhea (sometimes bloody, with mucus), pain in the abdominal region of varying strength and localization.
Intestinal colitis is a chronic disease with microscopic colitis, Crohn’s disease, ulcerative colitis. The causes of these diseases are not precisely clarified. The latest research suggests that the basis for the generation and development of intestinal inflammation is a combination of hereditary factors, the state of the intestinal microflora, dysregulation of the immune system and the environment. External circumstances that can trigger the disease include:
- use of antibacterial drugs;
- transferred intestinal infections in childhood and adolescence;
- food quality.
Acute intestinal colitis occurs when it is damaged by a specific infection, for example, salmonellosis, dysentery. In addition, intestinal colitis, occurring in acute form, is the debut of ulcerative inflammation of complex development.
Ulcerative colitis
Ulcerative colitis is a chronic inflammation of the colon and rectum. The disease is immune. The classification of pathology takes into account:
- The location of the inflammatory process. Proctitis ─ isolated damage to the end part of the intestine, left-sided colitis ─ inflammation spreads no further than bowing on the left side, total colitis.
- The nature of the disease. Acute ─ for 6 months from the debut of the disease, chronic recurrent ─ with an improvement of at least six months, continuous chronic ─ when there are no clearly defined periods of improvement.
- The severity of the exacerbation.
- The presence of complications.
- The response of the body to drug therapy.
Ulcerative colitis in acute form of the course is rare.
Causes
The causes of the disease are not fully understood. It is believed that it occurs as a result of a genetically determined disturbance of the immune system reaction, due to which immune cells attack the body’s own healthy cells, damaging the colon microflora. This is accompanied by inflammation, degenerative changes in the tissues of the digestive tract due to changes in the function of protecting the inner lining of the intestine.
Symptoms
Symptoms of ulcerative colitis: liquid stool with blood, imaginary urges, continuous pain in the rectum of a different nature ─ cutting, pulling, burning, and sharp urges to stool. Painful sensations in the abdominal region are less common and most often precede bowel movement. With a deep inflammatory process, the patient loses weight, feverish, weakness occurs.
In 75% of patients with ulcerative colitis of the intestine develops gradually. A person perceives the episodic appearance of blood in the stool as hemorrhoids. Therefore, sick people for a long time do not seek qualified medical assistance from a specialist.
The diagnosis is established after the examination of the intestine with an endoscope. An ultrasound examination (ultrasound) is performed as an additional diagnostic tool.
Treatment
When treating ulcerative colitis, a diet is prescribed, medicines are prescribed, and the patient is given psychological help. If indicated, surgery is performed. Patient management tactics are based on the following indicators: the activity of the inflammatory process, the volume of damage to the colon mucosa, the presence of extraintestinal signs of pathology, the duration of the disease, the results of previous treatment, and the risk of worsening the disease.
Proctitis
Patients with ulcerative proctitis with mild or moderately severe disease are advised to prescribe mesalazine (Salofalk) medication in the form of suppositories, enemas (rectal forms) at a dosage of 1 ─ 2 g per day. The effectiveness of this drug has been confirmed in 38 scientific studies. Suppositories (suppositories) for proctitis are preferable, since they ensure high saturation of the active substance in the zone of tissue damage. The introduction of drugs twice a day does not affect the outcome of the treatment relative to a single injection.
If the patient does not get better in the period from 10 to 14 days, glucocorticosteroid drugs (GCS) in the rectal form are added to the treatment at a dosage of up to 20 mg. The combination of GCS suppositories with mesalazine is also effective.
Total and left-sided colitis
Intestinal colitis in mild or moderate form of the disease is treated with mesalazine by oral administration (tablets), combining the introduction of the same medication in enemas. Sulfasalazine is also possible. This drug is also effective, but is slightly worse tolerated. If there is improvement within 2 weeks, therapy continues for 6 to 8 weeks.
The probability of remission is significantly increased (from 20 to 40%) in the case of prescription of mesalazine in the form of a multimatrix system (Mezavant preparation), providing a gradual release of the active substance and its even distribution throughout the large intestine, even if the drug is taken once a day. / p>
If there is no progress with therapy, intestinal colitis is treated with systemic glucocorticosteroid drugs combined with azathioprine. These drugs are also prescribed to support in case of remission. At the same time, it is important to carry out prevention of possible exacerbations.
With glucocorticosteroid therapy, its total duration is no more than 12 weeks. It is important to progressively reduce the dose of the drug, to control the level of glucose in the blood. For the main course of therapy, a combined medication is recommended to prevent the development of heart and kidney failure, and increase blood pressure. Assign vitamin D, calcium.
It is extremely important that when the symptoms disappear, observe the doctor’s prescriptions and continue maintenance treatment so that the colitis does not worsen.
Colitis of intestines with a complicated course is treated in a medical institution under the supervision of doctors – coloproctologists and gastroenterologists.
Surgical treatments for ulcerative colitis
With the ineffectiveness of drug therapy, surgical intervention is necessary. It is important not to delay the timing of the operation. Delay increases the risk of complications after surgery, then the disease is more severe.
The operation is inevitable in case of complications of the pathology: bleeding in the intestine, the risk of colorectal cancer, the detection of cancer. Such patients are usually 10 ─ 30%.
The best for ulcerative colitis is considered to be plastic restorative surgery – coloptectomy with an ileoanal reservoir anastomosis. A well-performed operation enables the patient to control the stool and defecate through the anus.
Forecast
Risk factors for severe course of the disease are early onset of the disease, the gradual spread of inflammation, and cases of intestinal colitis combined with liver disease ─ primary sclerosing cholangitis. The probability of a severe course of the disease throughout life is formed in 15% of patients. Total colitis increases the risk of worsening the inflammatory process. If adequate treatment is established for 5 years, deterioration of colitis avoids 50% of patients.
Some researchers consider the use of biliary ursodeoxycholic acid, which has anti-carcinogenic properties, as a promising but poorly studied method for preventing colon cancer. Several clinical and experimental studies confirm that prolonged use reduces the incidence of intestinal malignant tumors in patients with colitis.
Crohn’s Disease
Crohn’s disease is a chronic, recurring pathology of the digestive tract of unknown causes. Pathology is characterized by the progression of intestinal and general complications, lesions affecting all layers of the digestive tube. Crohn’s disease can damage the entire digestive system – from the mouth to the back opening, but more often – the intestines. In contrast to ulcerative colitis, this ailment is incurable.
Location of the lesion in Crohn’s disease:
| Terminal ileitis | Inflammation of the lower small intestine | ± damage to the upper part of the digestive tract |
| Colitis | Isolated inflammation of the colon and rectum | |
| Ileocolitis | Damage to the lower part of the small intestine and colon and rectum |
Inflammation of the upper part of the digestive system is almost never isolated. More often it proceeds with other forms of pathology.
Causes
Under the influence of external and hereditary circumstances, intestinal microflora and, possibly, not yet recognized microbiological agents, local immune defense is pathologically and continuously stimulated. This provokes the activation of the main cells of the immune system and other cells of the body. Pathological destruction of tissue occurs.
Colitis of the intestine occurs in a common and localized form, it is acute and its long course. The attacks of Crohn’s disease are mild, moderate and severe.
Symptoms
Options for the clinical expression of the disease are numerous. Colitis of the intestine manifests itself with the following symptoms:
- diarrhea, bloody diarrhea;
- pain in the abdominal region;
- weight loss;
- feverish states;
- iron deficiency anemia;
- anus lesions ─ inflammation of cellulose, cracks, fistulas (fistula);
- extraintestinal symptoms.
Severe Crohn’s disease occurs with external enteric-skin fistulas, internal fistulas, narrowing of parts of the digestive tube, obstruction in the intestinal tract, with intestinal bleeding.
Drug treatment for Crohn’s disease
Patient management tactics are based on the following indicators: the severity of the attack, the degree of inflammation of the digestive tract, the presence of extraintestinal symptoms, complications of the disease, its duration, the results of previous treatment, the risk of worsening the course of colitis.
The main objectives of therapy are to achieve stable remission, to preserve the previously obtained effect of treatment without glucocorticosteroid drugs, to avoid complications and operations.
Terminal ileocolitis, ileitis
Mild intestinal colitis is treated with budesonide ─ 9 mg per day for eight weeks. This is followed by a progressive reduction in dosage before discontinuation of the medication. Remission is supported by mesalazine. If there is no improvement, then middle-stage therapy is carried out.
At the middle stage of the disease, glucocorticosteroids (methylprednisolone or prednisolone) are prescribed in combination with drugs for artificial immunity suppression: 6-mercaptopurine, azathioprine, in the case of individual intolerance – methotrexate. With signs of improvement, the dosage of glucocorticosteroids is reduced.
If there are no shifts, prescribe biological treatment by acting on immunity with the medication adalimumab, infliximab, or decide to perform a surgical operation.
Crohn’s disease of the colon ─ colitis
Mild colitis attacks are treated with sulfasalazine or mesalazine. Clinical remission is supported by the same drugs.
At the moderate stage of pathology, glucocorticosteroids are prescribed, combining with drugs for artificially depressing immunity (immunosuppressors): 6-mercaptopurine, azathioprine, methotrexate.
The effectiveness of treatment with glucocorticosteroids is checked after 7 – 20 days. In the case of obtaining a good result, the administration of immunosuppressants continues, and the dosage of GCS is gradually reduced. In order to preserve the result obtained from treatment with drugs for artificially depressing immunity, their administration continues for 4 years.
Crohn’s Disease Attack
For a severe variant of the course of the disease of any localization in addition to the standard methods of treatment is carried out:
- antibacterial treatment;
- infusion treatment ─ leveling protein-electrolyte disorders, removing toxins from the body;
- correction of anemia ─ increase of hemoglobin level with iron preparations;
- nutritional treatment of debilitated patients.
If there is no change in treatment with intravenous glucocorticosteroids, a biological treatment is prescribed or an operation is done.
In the treatment of Crohn’s disease, prevention of infections arising from the weakening of the body and its defenses is performed. According to the European Treaty for intestinal colitis, patients must be vaccinated against hepatitis B, pneumococcal vaccine is introduced. Young women (under 25) are encouraged to be vaccinated against the human papilloma strain if it is not infected at the time of the examination.
Surgical treatment of Crohn’s disease
Virtually every patient with Crohn’s disease suffers at least one operation. Some patients undergo surgery more than once. During surgery for intestinal colitis, surgeons try to remove tissues with limited amount and, if possible, preserve organs.
Operations are prescribed for acute and chronic complications, when medications do not help, when the patient is lagging behind in physical development.
Colitis of the intestine is not cured even with the removal of all inflamed parts of the large intestine. Therefore, it is important to conduct supportive treatment, which begins as early as 12-14 days after surgery.
Forecast
Crohn’s disease is progressing. At the onset of the disease, complications are observed only in 15 ─ 20% of patients. After 10 years, complications are detected in 90% of cases. The operation 10 years after the debut of the disease suffers half of the afflicted. Many have bowel colitis after surgery.
Doctors call adverse factors for worsening the course of the disease widespread damage to the small intestine, colitis in children, inflammation in the anus, and smoking.
Extraintestinal symptoms of chronic colitis
The variety of clinical manifestations of Crohn’s disease, which are associated with the involvement of several organs of the digestive system at the same time, joining systemic (extraintestinal) manifestations make it difficult to recognize colitis.
Often the main clinical symptoms for a long time are extraintestinal colitis symptoms. They are not diagnosed as intestinal colitis, but as independent diseases. All therapy is directed to the treatment of extraintestinal diseases, and the underlying pathology continues to progress. In this regard, in most cases, Crohn’s disease is diagnosed on average 4 years after its onset. The precious time is missed for prescribing adequate treatment.
Numerous studies have identified an extraintestinal type of Crohn’s disease course, similar to appendicitis . The type of disease in which colitis of the intestine for a long time is expressed by only one sign, often extraintestinal, is highlighted. Among children, this may be growth retardation.
The number of complicated forms has increased. They occur in 35.4% of patients with intestinal colitis. Among them are the types of pathologies that manifest themselves:
- only extraintestinal (systemic) symptoms;
- specifically intestinal inflammation;
- a combination of intestinal damage and extraintestinal manifestations.
Some extra-intestinal complications depend on the activity of the intestinal lesion. They are curable and disappear as the main pathology is treated. Intestinal colitis provokes such diseases as:
- damage to the joints, in particular, arthritis of the upper and lower extremities;
- skin diseases ─ inflammatory nodes in the skin, skin necrosis;
- eye diseases ─ episcleritis, uveitis, iridocyclitis;
- fatty hepatosis ─ liver disease.
However, there are also systemic signs of colitis, which develop without regard to the inflammation of the intestinal tract:
- liver disease ─ primary sclerosing cholangitis;
- cholelithiasis;
- Joint disease spondyloarthritis, sacroiliitis.
Intestinal colitis remains a problem. The researchers are faced with the difficult task of Crohn’s disease: it is important to find the causes of the disease, understand the patterns of its development and find an adequate treatment regimen.
However, considerable information has been accumulated about each of the factors causing colitis. Despite the vagueness of the cause of Crohn’s disease, progress has been made in studying the mechanisms of its progression, treatment programs have been developed, and therapy methods are constantly being improved.
Microscopic colitis
Microscopic colitis is a chronic inflammation of the large intestine, the key feature of which is loose stools without blood. With this type of colitis, an X-ray conclusion and an examination of the intestine with an endoscope remain normal, traces of inflammation are detected only by a detailed analysis of the biomaterial obtained by colon biopsy (histology).
Causes
The mechanisms of formation of microscopic colitis are unknown. Literature data show the relationship of the disease with the pathological processes of the body’s defenses, bile acid absorption and smoking.
The basis of the disease may be the pathological reaction of the immune system of the epithelium of the colon. It is associated with the receipt in excess of bacterial, food, drugs. Immunity reacts to them as alien and attacks the healthy tissues of the body. A chronic inflammatory process develops.
Medication may play a provocative role in the occurrence of microscopic colitis:
- nonsteroidal anti-inflammatory drugs ─ antipyretic and analgesic drugs such as aspirin, ibuprofen, diclofenac;
- drugs in the treatment of diseases associated with increased production of hydrochloric acid in the stomach, ─ lansoprazole, omeprazole;
- drugs listed in paragraph 1 and 2, at the same time;
- third-generation psychotropic drugs for the treatment of anxiety disorders and depression.
However, the relationship between taking these medicines and inflammation remains poorly understood.
There are two types of microscopic colitis: collagen and lymphocytic.
Lymphocytic Colitis
Pathology is determined by a scattered increase in the number of lymphocytes of the mucous surface of the colon. The number of main cells of the immune system increases from 4.4 to 5.2 to 24 or more per 100 epithelial cells. The distribution of these cells in the intestine is uneven. They accumulate mostly in the dome of the cecum, the initial segment of the colon. On some segments of the mucous surface, desquamation and flattening of the epithelium occurs. The diagnosis is confirmed on the basis of typical changes in the tissues of the inner shell.
Lymphocytic colitis does not develop into malignant tumors. With careful medical research significant deterioration in the body is not detected. Only slightly increases the sedimentation rate of erythrocytes (ESR). The colon continues to function fully. Nutrient loss due to insufficient intestinal absorption is rare. Persistent continuation of loose stool occurs only in 7% of patients. Lymphocytic colitis can eventually transform into collagen colitis.
Collagen Colitis
Collagen colitis seals the collagen layer under the superficial epithelium of the colon. The gut thus becomes irregular in shape, it has irregular borders. As in the previous type of colitis, part of the intestinal mucosa is damaged, the content of lymphocytes and eosinophils also increases.
The causes of collagen colitis are also unknown. There is a version that the compression of the collagen layer occurs due to the disruption of the cells of the connective tissue (fibroblasts) as a reaction to stimulation by an unknown stimulus. Perhaps non-steroidal anti-inflammatory drugs can be an annoying factor. At the same time, approximately 5 years pass from the start of taking these drugs to the onset of symptoms. In medical practice, there was an episode of the formation of collagen colitis after the administration of simvastatin ─ medicine for the prevention of cardiovascular diseases.
Collagen colitis is often combined with endocrine diseases, which suggests its autoimmune origin ─ there is a pathological production of aggressive cells against the healthy tissues of the body. The disease is 10 to 20 times more common in women than in men. Colitis is acute in 35% of clinical cases.
Collagen colitis mainly occurs chronically, the risk of degeneration into a malignant tumor is unlikely. Significant degeneration of the mucous surface of the colon is absent. Occasionally, edema, a violation of vascular pattern.
Symptoms of microscopic colitis
The disease is formed more often after fifty years. In medical practice, there were cases of collagen colitis in a child.
Clinically lymphocytic and collagen colitis are indistinguishable. The leading sign of the disease is persistent watery diarrhea without blood, disturbing even at night. Stool frequency is usually 4 – 6 acts per day. But some people have stool up to 20 acts per day and decreases only when fasting. Watery stools provoke sudden, uncontrollable urge and fecal incontinence (40% of patients), especially at night.
Other signs of colitis:
- cramping acute pain, discomfort in the abdominal cavity;
- nausea, vomiting;
- flatulence;
- weight loss;
- inflammation of the joints ─ arthritis with inflammation of the wrist and joints of the lower limb.
The disease is variable. Colitis can be acute, chronic, with occasional exacerbations and long periods of sudden disappearance of symptoms of the disease.
Treatment of microscopic colitis
Colitis can be cured in 82% of clinical cases. But after completion of the main treatment phase, 60% of patients experience a relapse of the disease with the formation of a chronic course. This adversely affects the quality of life of the patient.
Approaches to the treatment of patients with lymphocytic and collagen colitis do not differ. The goal of treating microscopic colitis is to reduce the symptoms of chronic disease (remission) and improve the quality of life of patients.
Therapy is based on a consistent principle. First, drugs are canceled, in particular, nonsteroidal anti-inflammatory drugs, which may have contributed to the appearance of colitis. Diet is being discussed to exclude foods and drinks that aggravate stool disorder from the diet.
Antidiarrheal drugs are used, in particular, loperamide. But stable clinical remission in its use is rarely achieved, and a positive effect on colitis is unlikely. If the treatment is ineffective, it is advisable to prescribe cholestyramine. The drug binds in the intestines bile acids and microbial toxins, which provoke the development of diarrhea.
A second-line treatment for microscopic colitis is called bismuth subsalicylate. The drug relieves the symptoms of diarrhea, inflammation, has an antibacterial effect. Bismuth subsalicylate is taken at 0.35 g 3 times a day before meals. The course of treatment can last up to 2 months. However, long-term use of this drug, despite its proven efficacy, is limited due to side effects.
Six-month intake of mesalazine, alone or in combination with cholestyramine, leads to remission in 85% of patients with lymphocytic colitis and in 91% of patients with collagen colitis. The positive effect was more pronounced in cases of combination therapy. But a small number of patients respond to mesalazine.
The third line drug in the treatment of microscopic colitis is budesonide. This is a glucocorticoid, which has little effect on the entire body as a whole, unlike other steroid drugs. The drug is effective in the treatment of microscopic colitis. Taking budesonide for 6–8 weeks helps achieve remission in 80–90% of patients.
However, glucocorticoids inhibit the adrenal cortex, which produces hormones, and lead to its atrophy. There is a so-called steroid dependence. Therefore, budesonide is used only as a second or third line drug in the treatment of microscopic colitis. This drug also treats severe forms of the disease.
In severe microscopic colitis, drugs that artificially suppress the body’s immune system (immunosuppressive therapy) are prescribed: azathioprine, 6-mercaptopurine, methotrexate.
Surgical treatment of microscopic colitis is extremely rare, only in severe forms and in the absence of effect from any drug therapy.
Microscopic colitis is responsible for chronic diarrhea in 10 to 30% of cases. The first time the disease was described only in 1976, but it is not considered rare. Studies by modern epidemiologists suggest that the disease has progressed in recent decades.
Pseudomembranous (infectious) colitis
Pseudomembranous colitis is a disease of the colon in an acute form. It is caused by the spore-forming stick Clostridium difficile ─ CD. Clostridial infection is detected in patients taking antibiotics. The greatest risk of CD infection are patients of surgical and intensive care units, intensive care wards. Infection is transmitted by household from infected people to uninfected people through hands, care products, as well as through bedding, furniture, showers, toilets.
Causes
As a result of antibiotics, the healthy flora of the large intestine is disturbed, it is colonized with CD strains. They produce toxic substances that affect the inner lining of the colon and rectum. The colon is inflamed and damaged.
Infectious pseudomembranous colitis occurs after treatment with various antibiotics, including metronidazole and sulfonamides. But most often the clostridial infection is activated after the use of the following medicines:
- amoxicillin with clavulanic acid;
- clindamycin,
- cephalosporins II and III generation;
- fluoroquinolones,
- ampicillin.
Films (pseudomembranes) are a sign of this type of colitis. They are formed in the places of necrosis of the epithelial cells of the mucous membrane of the colon.
Symptoms
Pseudomembranous colitis is activated during antibiotic therapy or 10 days after the end of therapy. There is a late activation of the pathology up to 12 weeks after antibiotic therapy.
The main symptom of colitis is diarrhea. Sometimes diarrhea can be the only symptom. Sometimes the disease manifests itself in a feverish state. Episodes of liquid stool reach 5 times a day, and sometimes reach 20 – 30 acts of defecation. Watery diarrhea is characterized by a small amount, stool with mucus. Long-term diarrhea, may not stop for 8 ─ 10 weeks.
A mild course of pseudomembranous colitis is usually not detected: watery diarrhea is not accompanied by other symptoms. After the abolition of antibacterial drugs in 3-4 days diarrhea stops.
The moderate course of colitis is more intense. Discontinuation of antibiotics does not stop diarrhea. Frequent watery urges contain an admixture of blood and mucus. The disease is exacerbated: the temperature rises, symptoms of intoxication are observed: lethargy, fatigue, moderate reduction in blood pressure, nausea, vomiting, heart rate rises to 100 beats per minute. Pains in the abdominal region are exacerbated in front of the chair, the urge to be false.
Treatment
Therapy for pseudomembranous colitis includes stopping the intake of an antimicrobial drug associated with the cause of the pathology. Treatment of colitis is as follows:
- elimination of the strain CD in the intestine ─ prescription of drugs vancomycin, fidaxomycin;
- absorption and removal from the colon of infectious agents using the following drugs ─ polyphepan, cholesteramine, carbon sorbent, diosmectitis;
- restoration of intestinal microflora;
- elimination of dehydration.
When the patient has a colitis, a diet is prescribed – frequent meals in small portions, heavy drinking. Excluded are greasy, fried, spicy foods, fruit juices, carbonated drinks, coffee, alcohol.
The extremely severe form of the disease, the presence of symptoms of purulent inflammation in the abdominal cavity (peritonitis) require surgical intervention.
Radiation colitis
During radiotherapy for oncological diseases of the abdominal cavity, small pelvis and genital organs, radiation to various parts of the small or large intestine occurs simultaneously. Therefore, in 10–15% of patients early or late radiation lesions of a different nature are formed.
Radiation damage to the colon at an early stage is associated with the specific effect of ionizing radiation on the mucous surface. This leads to colitis. Radiation damage at a later stage is associated with damage to the small vessels of the submucosal layer of the colon. This is accompanied by a violation of blood circulation. As a result, the intestinal mucosa gradually atrophies, ulcers and erosion occur.
Symptoms
The early stage of colonization with ionizing radiation progresses in a three-month period after radiation therapy. The signs of radiation colitis are similar to the clinical signs of other inflammatory diseases of the colon. Over time, the inflammation may go away.
In case of a more severe course of the disease after the end of radiotherapy or immediately after the patient is irradiated, vomiting occurs. Cancer patients lose weight, they have no appetite, abdominal pain, and diarrhea. The activity of colitis depends on the dose of ionizing radiation, the localization of the pathological process.
The late stage of colon damage begins to progress at 4 ─ 12 months after radiotherapy. The initial symptom is discomfort associated with a disorder of stool of a different nature ─ persistent constipation or frequent diarrhea with false desires. Feces may be mixed with mucus or blood. Other symptoms of colitis are pain in the abdominal region of varying intensity, nausea, loss of appetite. The patient loses weight.
Treatment
Intestinal colitis associated with damage due to ionizing radiation is treated the same way as ulcerative colitis, Crohn’s disease.
Drug treatment lasts a long time. Therapy is carried out by glucocorticosteroid drugs (budesonide), prescribed pentasu, salofalk, mesalazine – 5-aminosalicylic acid preparations.
Special attention is paid to the patient’s diet:
- high protein content, a certain amount of carbohydrates, fats, minerals and vitamins;
- food must be mechanically processed, without tough plant fiber;
- sparing food without smoked products, seasonings, marinades, pastry products;
- Limit or exclude milk and dairy products.
The intestinal epithelium is restored by etadeno, sea buckthorn or rosehip oil (by mouth 2 hours before meals). In case of diarrhea, antidiarrheal drugs are used ─ loperamide (imodium), enterosgel, smecta, it is recommended to drink sweet jelly from cherry fruit or blueberries, decoction of pomegranate crusts.
Correction of dysbiosis is carried out, prescribing the bacterial drugs Linex, bifiform, baktisubtil. Digestive processes in the intestine are stimulated with penzital, pancytrate, mezim, panzinorm, and creon enzyme preparations.
Ischemic Colitis
With circulatory disorders of the abdominal aorta, ischemic colitis occurs. There may be two reasons provoking the development of this disease:
- artery disease ─ abnormalities in the development of blood vessels, elevated cholesterol levels, damage to blood vessels due to nervous regulation disorders;
- extravascular compression of the aorta of the abdominal cavity.
Due to insufficient admission to the intestinal arterial blood, surface death of epithelial cells occurs, the number of mucus-producing cells decreases, focal accumulations of cellular elements with blood and lymph are formed, and intestinal motor activity decreases. These changes lead to stagnation of fecal masses, blockage of the vascular bed. There is colitis.
Symptoms
Violation of intestinal circulation can be acute and in the chronic stage. The main symptom of chronic ischemic intestinal colitis, doctors call pain after eating in the intestinal area. The pain provokes insufficient blood flow to the organs of the gastrointestinal tract during digestion and the sensitivity of the intestine to this fact. At the initial stage of the development of the disease, pain is defined as a feeling of heaviness in the abdominal region. With the increase in circulatory disorders, the pain becomes dull, its strength begins to increase.
Another common symptom of chronic colitis is bowel disorder: persistent constipation, diarrhea, flatulence, unstable stool.
Violation of the work of the intestines, constant pain force a person to eat less. Progressive weight loss is another symptom of chronic ischemic colitis.
Based on the research, microscopic ischemic colitis is isolated. It is formed in the elderly in those who suffer from pathological disorders of the cardiovascular system. Typical signs of microscopic ischemic colitis are pain in the abdominal region, mostly in the left side between the lower rib and the pelvic bone, which are activated after eating, stool retention, flatulence, abdominal discomfort.
Treatment
Tactics of drug treatment depends on the depth of manifestation of chronic ischemic colitis, its stage. Doctors recommend strict adherence to the diet:
- proteins ─ 10 – 15%;
- fats of plant origin ─ 25 – 30%;
- polysaccharide carbohydrates ─ 55 – 60%;
- a high fiber diet.
Food for colitis should be in small portions, fractional.
Prescribed drugs to prevent the reduction of cardiovascular exacerbations: simvastatin, fluvastatin, atorvastatin. However, the return from taking these medications occurs only after 7–8 months from the start of therapy. Patients with severe atherosclerosis are prescribed a combination of these medicines with ezetimibe.
For the prevention of functional disorders of the liver, Essentiale, Essliver Forte, Phosphogliv courses are prescribed several times a year. In order to prevent thrombosis, take Fraxiparin.
To prevent pain, with the planned treatment of disorders of the chair during colitis, antispasmodics are prescribed – Drotaverine, Mebeverin (Duspatalin). Flatulence is effectively treated with meteospasmil. Against constipation, lactulose (Duphalac) is prescribed to older people. When taking it, there is no need to additionally drink liquid, the drug does not provoke addiction, it can be taken by diabetics, it is effective for liver diseases.
To restore the intestinal microflora with colitis, the colon is treated by metronidazole, Alpha Normix. Medicines are taken for 8 – 10 days, then they are prescribed probiotics Bifiform, Probifor or Linex . Surgery is also performed in the treatment of ischemic colitis.
Over the past three decades, the course of colitis has changed. Acute forms of ulcerative colitis are less common, and the number of chronic forms has increased. The frequency and prevalence of this pathology continues to grow, the course and severity of complications progresses. The question of how to treat intestinal colitis, how to diagnose it in the early stages, concerns not only domestic, but also foreign specialists. Researchers have stepped up activities aimed at studying the disease.