Chlamydia is a dangerous and common infectious disease. She can get sick of people of different ages and genders, but more often she affects young people. And this is not surprising, because in most cases the disease is sexually transmitted.
Why the disease is dangerous for women
Too many women are unaware that they are sick, because the disease is often asymptomatic. Accurate statistics about the incidence of chlamydia does not exist. However, this disease is much more common than other venereal diseases.
According to various estimates, the number of women with this disease varies from 8% to 40%, and their total number on Earth is about 1 billion. Therefore, the chance of being infected with chlamydia is very large. And, therefore, you need to know well what it is – chlamydia, its main symptoms, how chlamydia manifests itself in women, and how to treat chlamydia in women.
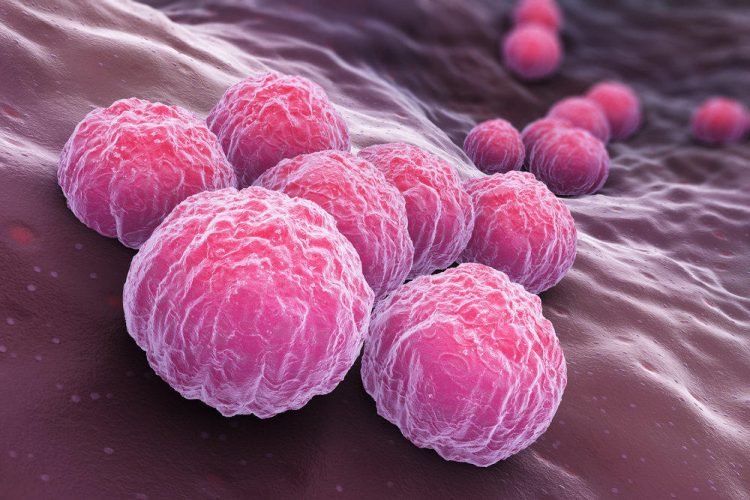
Description of the disease
Chlamydia is caused by the bacterium Chlamydia trachomatis. Chlamydia is a very interesting microorganism from a scientific point of view. Despite the fact that chlamydia trachomatis belongs to the realm of bacteria, nevertheless, it has certain features that bring it closer to viruses. Chlamydia – intracellular bacteria, they are able to infect body cells and reproduce directly in them. Bacteria cannot produce some of the enzymes necessary for their livelihoods. To do this, microorganisms penetrate into the cells of the human body, and take from there all that is necessary. Thus, chlamydia trachomatis are intracellular parasites.
Bacteria, however, can live in the extracellular space. When chlamydia enter the living cell, they acquire the ability to divide, increase in size and turn into the so-called reticular form. In this form chlamydia multiply. After the formation of new bacterial cells, they leave the host cell, and it dies. This whole process takes 2-3 days. And the bacteria, in turn, are sent in search of new victim cells. As the disease progresses, it takes on a chronic form, and the bacteria capture not only the lower, but also the upper parts of the urogenital system.
Chlamydia is fairly resistant to adverse effects and can exist in room conditions for up to two days. The incubation period for chlamydia is 2 to 4 weeks.
The main method of infection is considered sexual. In this case, infection with chlamydia can occur both during vaginal and anal sex, as well as during oral contact. In addition, some scientists tend to believe that bacteria are capable of being transmitted through the household, through the use of common objects, but this happens infrequently. Another way to transmit bacilli is from mother to newborn baby. It is not yet clear whether chlamydia can enter the baby’s body directly through the placenta. However, it has been proven that infection of the fetus can occur in a mother with chlamydia. A common route of infection is the birth process, in which the child passes through the mother’s birth canal infected with chlamydia. Usually, a child has chlamydial conjunctivitis (in 50% of cases). More rarely, pneumonia can occur, but it is even more dangerous.
Contrary to popular belief, chlamydia caused by Chlamydia trachomatis is not transmitted by airborne droplets. Although there is such a disease as chlamydia pneumonia or respiratory chlamydia caused by another type of chlamydia and which can be transmitted in a similar way.
It is also quite difficult to get infected with the help of kisses, since for this, there must be a very high concentration of bacteria in the mouth cavity of the partners, which is found only in advanced forms of systemic chlamydia.
Symptoms of Chlamydia in Women
When microorganisms enter the body, at first the symptoms may be hardly noticeable or not visible at all. This feature is more characteristic for women than men. In women, chlamydia similarly occurs in 70% of cases.
Signs of chlamydia can include a rise in temperature. This usually occurs soon after infection. The temperature rises to subfebrile values - + 37-37.5 ºС (98.6-99.5 ºF), fatigue and weakness may appear. However, later the temperature may drop to normal values.
In chlamydia, symptoms are usually associated with the condition of the urinary organs. The cervix, fallopian tubes, appendages, the endometrium, the Bartholin glands, the urethra, the vagina, and the bladder are not a complete list of the objects that chlamydia affects. This leads to inflammation of the urinary organs, more precisely, their mucous membranes. Chlamydia can also lead to the formation of adhesions in the abdominal cavity, which is fraught with sterility.
Signs of chlamydia can include small pains of the pulling type in the lower abdomen, itching, burning, cramping when urinating, feeling of increased humidity in the genital area, frequent urination, menstrual disorders, back pain. However, many women are not inclined to pay attention to these symptoms or to associate them with any other reasons.
But one of the main symptoms of chlamydia is the appearance of unusual secretions from the genitals. Chlamydia secretions have an abnormal appearance. Usually they have a whitish or yellow color, mucopurulent consistency and an unpleasant smell.
Chlamydia Consequences
However, chlamydia is much more dangerous than it seems at first glance. Chlamydia can have a number of unpleasant complications. As it develops, other tissues of the body – teeth, joints, eyes, and even the heart – may also be affected by chlamydia. For women who are infected with chlamydia, Reiter’s syndrome is characteristic, with arthritis, conjunctivitis and inflammation of the vagina.
There is a risk of severe lesions of the urinary system – urethritis, purulent cystitis, narrowing of the urethra. Chlamydia can also cause Fitz-Hugh-Curtis syndrome, which is characterized by simultaneous inflammation of the peritoneum (peritonitis) and liver capsules.
But chlamydia is most dangerous for pregnant women. Infection can cause complications of pregnancy, including ectopic pregnancy, polyhydramnios, and lead to early termination of pregnancy or missed abortion. Chlamydia can also be provoked by such phenomena as premature labor and prematurity of the fetus.
If the baby is still born at the appropriate time, then as a result of infection by bacteria (in the womb or during birth), it may develop inflammatory diseases such as conjunctivitis and otitis. In the future, the presence of bacteria in the body of a child can lead to problems with the cardiovascular and nervous systems, the gastrointestinal tract. For girls, infection in infancy threatens with further infertility.
A serious complication of chlamydia is cervicitis – inflammation of the cervix, cervical zrosia, and endometriosis – damage to the endometrium. They can lead to further sterility.
For these reasons, treatment should not be delayed, since the disease is easier to treat at an early stage.
Diagnosis of Chlamydia
For signs of chlamydia, even if there is only a suspicion of the disease, you should consult a doctor. A number of diagnostic measures are required to identify the infection. First of all, it is a visual inspection by a gynecologist. It will help to determine the lesions of the mucous membranes of the genital organs and the pathology of the cervix uteri that are characteristic of infectious diseases.
Also informative is the analysis of the patient’s history, the presence of gynecological problems in her past. There are several diseases in which there are significant reasons to suspect chlamydia:
- infertility (for a year or more)
- cervicitis,
- complicated pregnancy (high water, delayed fetal development, threatened miscarriage).
If such problems are detected, even if a smear on bacteria from the vagina does not show the presence of pathogenic microflora, the patient needs to undergo a thorough examination. Practice shows that the probability of identifying the pathogen is high enough – about 80%.
In patients, it is not always easy to determine the fact that the causative agent is Chlamydia Trachomatis, and not some other microorganism. In particular, the discharge in chlamydia is similar to those seen in other diseases – herpes, gonorrhea, etc. However, there are methods that make pathogen detection possible.
The most accurate is a test for the detection of chlamydia using particles of bacteria DNA bacteria – a test using the polymerase chain reaction (PCR). In the presence of a pathogen in a patient, it gives an almost one hundred percent result. Other types of studies can also be conducted, for example, fluorescent detection of pathogens (immunofluorescence, enzyme immunoassay). The probability of detection of bacteria in this method is 50%.
A culture in bacteria is also carried out in a nutrient medium (the probability of detection of the pathogen is 70%) and the search for antibodies in the blood is a serological test. A smear from the vagina can also reveal a chlamydial infection. However, with this method, the probability of detecting bacteria is low, at 15%.
In addition, ultrasound can be used to detect changes in the tissues of the reproductive organs that are characteristic of chlamydia. The sooner the disease is diagnosed, the greater the chances of a successful cure of the disease.
Treatment for Chlamydia in Women
Treatment for chlamydia is a complex process. The main method is antibacterial therapy. Fortunately, the pathogen has a high sensitivity to many antibiotics. But not all. In addition, antibiotic treatment requires not only choosing the right type of drug, but also determining its correct dosage, taking into account the patient’s immunity, its concomitant diseases, including the possible presence of other sexually transmitted infections. Comprehensive analysis of these factors is not an easy task. Therefore, self-treatment of chlamydial infection with antibiotics is unacceptable. It can lead to a deterioration of the patient’s condition and to the fact that the disease becomes chronic intractable form.
Therapies typically use drugs from the group of macrolides (azithromycin, josamycin, clarithromycin, spiramycin), penicillins (ampicillin) and tetracyclines (tetracycline, doxycycline). Fluoroquinolones (levofloxacin, ciprofloxacin, norfloxacin, lomefloxacin, sparfloxacin) are used as reserve drugs used for the ineffectiveness of standard drugs. Usually, if bacteria are resistant to one drug, then drugs from another group of antibiotics are used.
In particular, azithromycin shows high efficacy. In general, a single use of this drug in the amount of 2 tablets is enough to destroy all chlamydia in women in the body. Or the following scheme can be used – on the first day, 500 mg of the drug is taken, and in the next four days – 250 mg each. However, this drug is contraindicated in pregnancy.
Doxycycline is usually taken in a dosage of 0.1 g 2 times a day during the week. This drug is also contraindicated in pregnancy. In the standard case, the course of treatment with ampicillin is 250 mg 4 times a day for 10 days.
Selection of drugs during pregnancy requires special care, since many of them are not recommended in this period due to high toxicity. Usually, therapy is best done during the second trimester, after the formation of the placenta. Most commonly, erythromycin and josamycin are used during pregnancy. The duration of treatment during pregnancy is usually shorter.
However, antibiotics are not the only essential drugs. Depending on the condition of the patient, the doctor may also prescribe drugs to stimulate the immune system and vitamin complexes. Also, the disease is often complicated by a secondary fungal infection of the genital organs, such as candidiasis. Therefore, antifungal agents (Fluconazole, Nystatin) may be prescribed for its treatment.
It is important to note that in the event that a permanent sexual partner is also infected, it is necessary to simultaneously treat it. Otherwise, all efforts to get rid of bacteria will be useless, because the next sexual contact will lead to re-infection. It should be borne in mind that the body does not produce specific immunity against bacteria, and having had the disease once, the second time, it can be picked up with the same ease. The presence of diseases such as urethritis or prostatitis in a man indicates that he is also likely to be a carrier of chlamydia.
It is also worth noting that for the period of treatment it is necessary to refrain from sex with a sexual partner, no matter whether it is a healthy partner or a patient. This situation should last until it becomes obvious that both partners no longer have pathogens in the body.
To check the effectiveness of therapy after it is completed, control studies are conducted for the presence of pathogens. Usually studies are conducted after two weeks, a month and two months.
Antibiotic therapy should also be accompanied by a course of treatment for dysbacteriosis associated with antibiotics. For this purpose, probiotic preparations may be prescribed.
In addition to taking general antibiotics, local antiseptic preparations can be used, such as chlorhexidine solution. With the defeat of the urinary organs, these drugs can affect the causative agent of the disease. These drugs may be contained in vaginal suppositories and ointments. You can also use trays, tampons, microclysters.
There are also drugs containing bacteriophages active against the pathogen – Kolifag, Intestitis bacteriophage. In some cases, various physiotherapeutic procedures can be prescribed as an auxiliary measure of therapy – radiation by ultrasound and laser, magnetic therapy, electrophoresis. An important element of treatment is diet. During the course of therapy, it is recommended to abandon too spicy and sweet foods, alcohol.
Prevention
There are no vaccines to protect against trachomatis bacteria, therefore, in order to avoid illness, certain rules must be followed to minimize the risk of infection by the pathogens.
Disease prevention largely coincides with the prevention of other sexually transmitted diseases. First of all, this is the use of barrier contraceptives. However, this method is not a panacea, as it does not exclude infection. Interestingly, oral hormonal contraceptives also reduce the likelihood of infection, as they make the uterine lining more resistant to bacteria.
It is equally important to avoid promiscuous sex, frequent change of partners, unconventional, anal and oral sex. You should also monitor personal hygiene, wash hands, especially after going to the toilet, public places. The probability of transmission of the pathogen through such things as common towels, clothing, especially underwear, etc., is very high. These points should be considered to prevent infection of other family members. Therefore, it is necessary to have individual means of hygiene – towels, washcloths, sponges, etc.
Since the disease has a tendency to asymptomatic course, then if you have regular sex life and different partners, you must undergo an annual examination.